Not an End, But a New Beginning: Empowering Yourself as a Breast Cancer Survivor
For many women, the last day of breast cancer treatment is one filled with relief and hope. Yet it can also feel unexpectedly unsettling. Survivorship isn’t the end of a story, but the beginning of a new chapter—balancing ongoing medical care with healthy habits, emotional honesty, and resilience [1].Survivorship is not about going back to who you were before. It’s about reclaiming the control that cancer disrupted and moving forward into the person you are becoming [2]. Taking Steps Towards Health and Healing
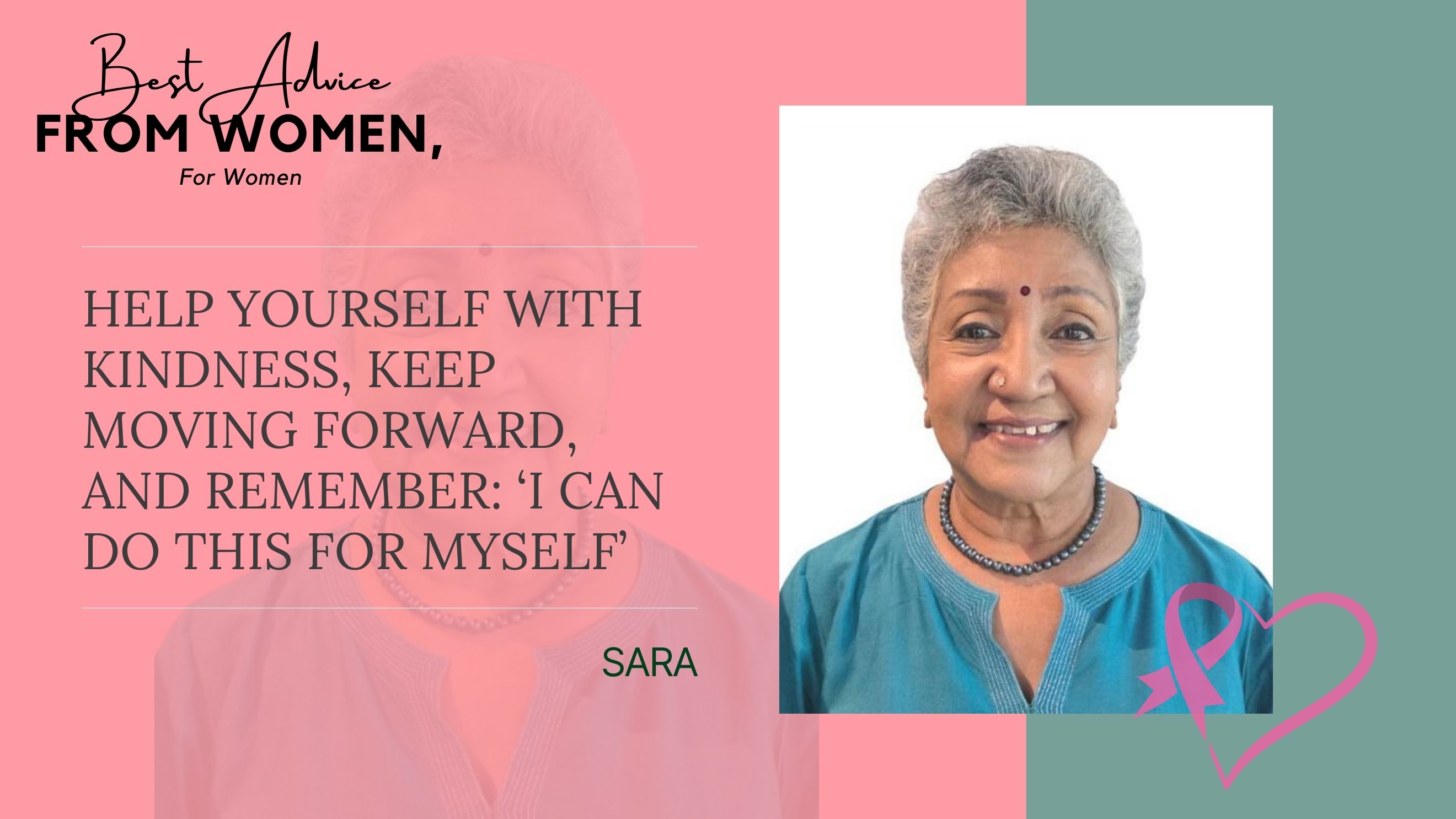
“I want to take charge of my health.”After treatment, your healthcare team may recommend follow-up visits to monitor for recurrence or secondary cancers [2] [3]. These appointments can stir up anxiety, but they are also opportunities to ask questions, share symptoms, and feel more in control. [1] [4] [5]. Tip: Write down three questions before each follow-up visit. This can help you focus on what matters most and ease uncertainty.Beyond check-ups, daily habits play a powerful role in recovery. Physical activity has been shown to lower anxiety and depression, boost well-being and help reduce the recurrence risk [5] [6] [7]. Nourishing your body with a fibre-rich foods, fruits, vegetables and whole grains supports long-term health [5].Empowerment isn’t about forcing positivity. It’s about acknowledging when you’re struggling, giving yourself compassion, and still choosing steps that nurture your healing [8].Adjusting to Your New Normal
“Life feels different now, and that’s okay.”Many survivors long to “get back to normal,” but life after cancer rarely looks the same [9]. Physical changes like surgical scars, early menopause or fatigue may leave you feeling disconnected from your body [9]. Emotionally, the fear of recurrence or grief for pre-cancer self can weigh heavily [1] [9]. These shifts can ripple into relationships too. Loved ones may expect you to bounce back quickly, which can feel isolating [1] [2]. The first step in navigating these changes is permission—permission to acknowledge these challenges honestly. Healing isn’t linear; it’s more like the tide, flowing in and out. With time, small steps toward your own “new normal” can help you feel more grounded [10].Redefining Yourself and Finding Confidence
“I’m not who I was before.”For many, survivorship becomes a chance to rewrite their story. Cancer may reshape body image, sexuality, routines and even career paths, but it also sparks new perspectives [11] [12]. This period is often described as rediscovery—finding strength you didn’t know you had, deepening relationships, and noticing meaning in everyday moments [1] [2] [4]. Not everyone feels comfortable with the label “survivor”, and that’s okay[1] [2]. Identity after cancer isn’t about erasing what happened. It’s about weaving those experiences into your new narrative—one that reflects both the scars you carry and the confidence you are building. Finding Strength Through Community and Support
“I can’t do this alone, and I don’t have to.”Healing is strongest when shared. Social support, whether from family, friends, survivor groups or your care team, can ease stress, strengthen emotional adjustment and improve well-being [2] [6] [13]. Many women find comfort in survivor groups where others truly understand their journey. These conversations can bring hope, practical coping strategies, and a sense of belonging [2]. At the same time, leaning on close relationships can help rebuild trust and connection, even if cancer has shaken old support systems [13].Empowerment doesn’t mean facing everything alone. It also means knowing when to lean on others. Survivorship is both individual and collective, and walking this path together can make each step feel lighter.Moving Forward with IntentionEvery small step—whether speaking up about side effects, starting a new health habit, or reaching out for support—is part of reclaiming your strength.While it’s natural to grieve the life you had before, remember this: you are more than the scars cancer has left behind. At Solis and Luma, we believe the end of treatment is not the end of the cancer journey. Survivors deserve continued care, compassion, and tools to live fully and earnestly after cancer. The Breast Years of Your Life: Living Well After Cancer offers practical guidance and heartfelt support - from rebuilding trust with your body to embracing new beginnings -so you can continue to live meaningfully beyond cancer. References[1] Cancer Council, Living Well After Cancer [2] European Society for Medical Oncology, The Guide for Patients on Survivorship [3] Cleveland Clinic, Cancer Survivorship [4] Mayo Clinic, Cancer survivors: Managing your emotions after cancer treatment [5] Solis Breast Care & Surgery Centre, The Breast Years of Your Life: Living Well After Cancer [6] BMC Women's Health, "Resilience and renewal: the personal impact of physical activity in breast cancer survivors" [7] American Cancer Society, Physical Activity and the Person with Cancer [8] American Cancer Society, Life After Cancer [9] Journal of Cancer Survivorship, "Psychosocial experiences of breast cancer survivors: a meta-review" [10] Asia-Pacific Journal of Oncology Nursing, "Perceived New Normal and Inner Strength on Quality of Life in Breast Cancer Patients Receiving Adjuvant Endocrine Therapy" [11] National Cancer Institute, Life After Cancer Treatment [12] Latin American Journal of Palliative Care, "The (re)construction of female identity among women cancer survivors" [13] Asia Pacific Journal of Cancer Prevention, "Importance of Social Support in Cancer Patients"